For more than 50 years, a network of public programs and providers have assisted millions of reproductive age (18 to 49) women with low incomes in the U.S. to obtain sexual and reproductive health services. Over the past decade, the landscape of reproductive health care has changed dramatically as a result of shifts in federal and state policy as well as legal challenges and court rulings that have reshaped the state and federal laws that govern these programs. Recently, the 2025 Budget Reconciliation Law prohibits federal Medicaid payments for one year to some family planning providers that also offer abortion services, and the President’s most recent budget request proposes to eliminate funding for the federal Title X family planning program. This brief explains the major sources of public financing for family planning care, related policies, and their role financing services for low-income women.
Family Planning Services
Family planning encompasses a wide range of counseling, prevention, and treatment services that nearly all women use during their lifetimes. Contraceptives are the primary service, which most women use over the course of their lifetimes. Many options are available from clinicians including permanent methods, long-acting methods such as IUDs and Implants, as well as pills, injectables, patches, and rings. Over–the-counter methods include condoms and emergency contraception pills and more recently, Opill, a daily oral contraceptive pill. In addition to contraceptives, family planning includes sexual health services such as STI testing and treatment, gynecologic exams, and pregnancy testing (Figure 1).

Financing Family Planning Services for Low-Income People in the U.S.
Financing reproductive health care for people with low incomes comes primarily from a variety of public programs, including Medicaid, the federal Title X Family Planning Program, Section 330 of the Public Health Service Act (PHSA), and the Indian Health Service. Clinics and other providers may receive funds from a combination of these programs, which are described below.
Medicaid
Medicaid is a health coverage program for individuals with low incomes that covers more than 15 million reproductive age women nationally. Like private insurance, Medicaid pays clinicians and clinics for health services they provide to their patients. Jointly operated and funded by the federal and state governments, Medicaid provides health coverage to one in five women of reproductive age and more than four in ten (44%) who have low-incomes (Figure 2). The share of low-income reproductive-age women enrolled in Medicaid varies considerably by state, ranging from a high of 34% in Louisiana to a low of 10% in Utah. These differences are the result of a variety of factors, including demographic differences between states such as the share of women with low incomes, availability of employer-sponsored insurance, state choices about Medicaid eligibility, particularly whether the state has expanded Medicaid to all adults up to 138% FPL as permitted by the Affordable Care Act (ACA) and state-established income eligibility thresholds for parents in the non-expansion states. For these women, Medicaid provides comprehensive affordable coverage to help meet the full range of their health care needs, including family planning services.
Because it covers so many people, Medicaid is the largest source of public funds for family planning services. Federal law stipulates that family planning is a “mandatory” benefit that states must cover under Medicaid, but states have considerable discretion in specifying the services and supplies that are included in the program. Additionally, the ACA requires most private insurance plans and Medicaid expansion programs to cover the full cost of prescribed contraceptive methods for women. Most state Medicaid programs cover the full range of FDA approved contraceptives available to women, counseling and treatment for STIs and HIV, and screening for cervical cancer. Medicaid reimburses clinicians for delivering family planning care, just as it pays for other medical services.
Abortion services are not considered to be family planning, and the Hyde Amendment prohibits any federal dollars, including Medicaid reimbursements, from being used to pay for abortion care except in cases of rape, incest or life endangerment of the woman. Other federal requirements that shape family planning policy under Medicaid include:
- Federal Matching rate – The federal government pays 90% of all family planning services and supplies, which isconsiderably higher than the federal match that states receive for most other services for the traditional Medicaid population, which ranges from 50% to 78%, depending on the state. The federal government also picks up 90% of the costs for all services among the expansion population.
- Ban on cost sharing – Federal law prohibits cost sharing for any family planning (and pregnancy-related) services.
- Freedom of choice – The federal Medicaid Act states that beneficiaries have “freedom of choice” to obtain family planning services from any qualified provider participating in the program, but recent policy decisions (discussed below) are changing this.
- Managed care –Nationally, nearly three in four (74%) reproductive age women with Medicaid are enrolled in managed care plans. While access to most services may be limited by managed care networks, federal law states that for family planning services, enrollees may seek care from any Medicaid provider even if the provider is outside of the plan’s network.
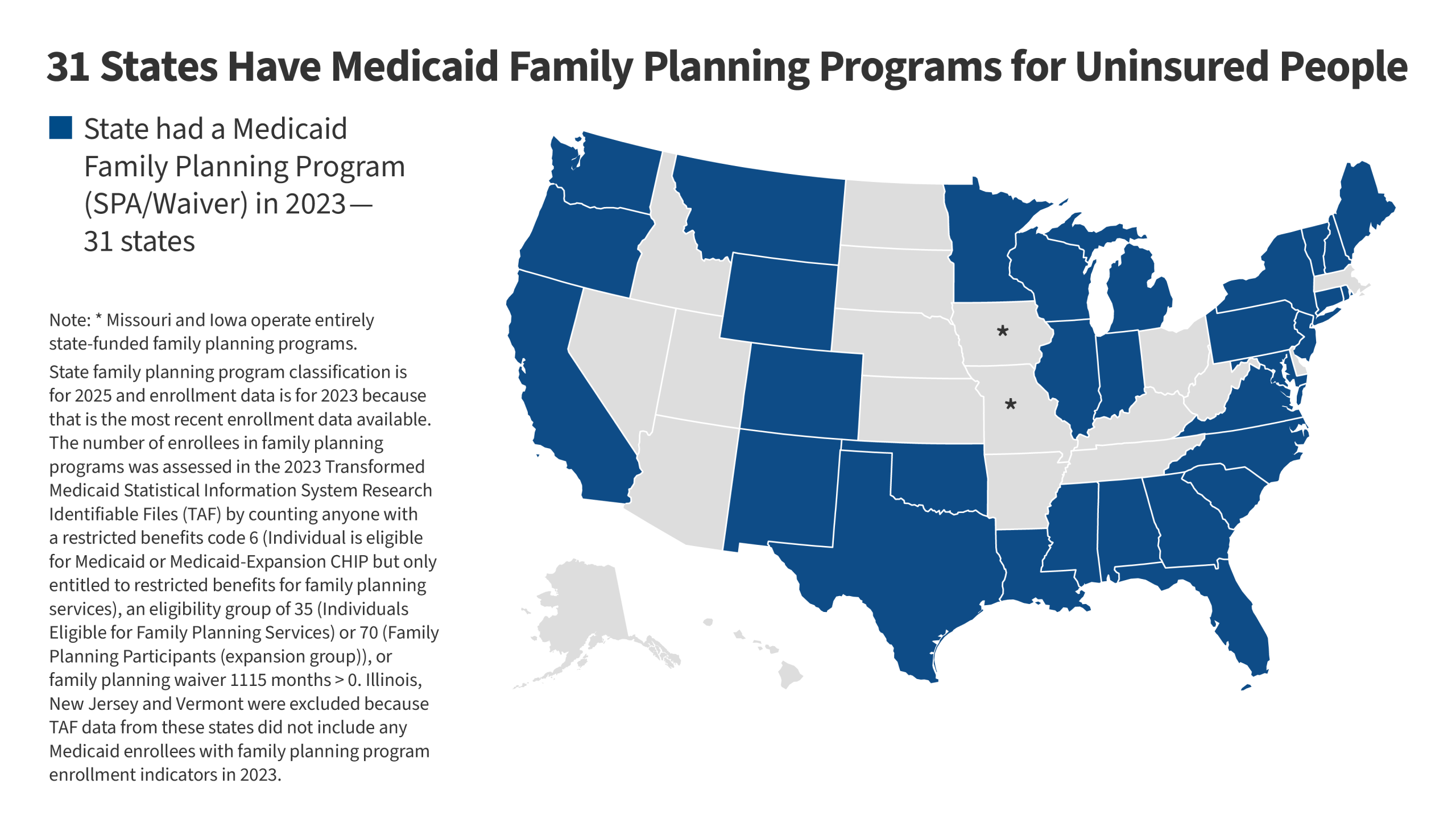
- Family planning specific programs – States may establish limited scope programs through Medicaid Section 1115 Research and Demonstration Waivers or through State Plan Amendments (SPAs) to provide coverage for family planning services only to individuals who do not qualify for full-scope Medicaid. Today, more than half of states have established such programs (Figure 3).
Free Choice of Provider and Medicaid
Historically, the federal Medicaid statute has required states to allow all willing and qualified providers to participate in their Medicaid programs. States were not permitted to exclude or disqualify providers just because they offer abortion services in addition to preventive family planning services. However, a Supreme Court ruling and a new federal law in 2025 have upended this requirement.
- In Medina v Planned Parenthood of South Carolina, a 2025 decision issued by the Supreme Court ruled that Medicaid enrollees cannot seek relief in federal court to enforce Medicaid’s “free-choice of provider” provision and that the law does not confer rights to individual enrollees. This limits the ability of Medicaid enrollees to challenge state decisions on disqualifying clinics from the Medicaid program. It effectively allows states to disqualify providers because they offer abortion services in addition to family planning care, upending a longstanding federal protection. This has had an immediate impact on Planned Parenthood clinics in South Carolina but also is expected to be used by other states to block Planned Parenthood from participating as a Medicaid provider.
- Another major national change in Medicaid stems from a provision of the federal budget law, enacted in July 2025. The law blocks federal Medicaid payments to certain clinics that offer both abortion and family planning services for one year starting July 4, 2025. It specifically affects Planned Parenthood clinics across the country as well as clinic networks in Massachusetts and Maine. The provision has been challenged by multiple lawsuits, yet it is in effect and clinics are not being paid with federal funds for family planning services they provide to Medicaid beneficiaries for one year, losing a major source of revenue. Some clinics state they will have to close, make major reductions in services, or stop seeing Medicaid enrollees as a result.
Title X Program
The Title X National Family Planning Program, a federal block grant administered by the HHS Office of Population Affairs (OPA), is the only federal program specifically dedicated to supporting the delivery of family planning care. The program funds organizations in each state to distribute federal dollars to safety-net clinics to provide family planning services to low-income, uninsured, and underserved people. In 2023, approximately 4,000 clinics nationwide received Title X funding, including specialized family planning clinics such as Planned Parenthood centers, primary care providers such as federally qualified health centers (FQHCs), and health departments, school-based, faith-based, and other private nonprofits. In 2023, 60% of clients seen at Title X clinics had family incomes at or below the poverty level, almost half (46%) were covered by Medicaid or another public program, and more than a quarter (27%) were uninsured (Figure 4).
Signed into law by President Nixon in 1970, the Title X program’s funding has remained flat at $286.5 million for the past ten years. In addition to providing clinics with funds to cover the direct costs of family planning services and supplies such as contraceptives, Title X funds enable clinics to pay for patient and community education services about family planning and sexual health issues, as well as infrastructure expenses such as rent, utilities, information technology, and staff salaries. Clinics that receive Title X funds are also eligible to obtain discounted prescription contraceptives and devices through the federal 340B program. No other federal program makes funds available to support clinic infrastructure needs specifically for family planning. Clinics that receive Title X funds also receive Medicaid and private insurance reimbursements for specific clinical services they provide to enrollees with coverage. Title X grantees cannot charge patients with low incomes out of pocket for services they receive, and for people with annual family income above 250% FPL, charges should be on a sliding fee schedule based on ability to pay.
Title X regulations have historically stipulated that participating clinics must provide clients with a broad range of contraceptive methods as recommended by the national Quality Family Planning Guidelines (QFP), and ensure that the services are voluntary and confidential. This has been interpreted to mean that minors do not require parental involvement to obtain family planning services as a Title X funded site. The current QFP guidelines serve as standards for delivery of clinical sexual and reproductive health services and address a range of issues, including STIs, fertility, and gender-affirming care. Federal rules also require that participating clinics offer their patients non-directive pregnancy options counseling that includes abortion, adoption, and prenatal referral for those who seek those services. These requirements, however have changed with different presidential administrations shaping who can participate and what services can be offered.
Site of Care for Sexual and Reproductive Health for People with Lower Incomes
Most reproductive age women obtain reproductive care from a private doctors’ office; however many women with lower incomes get family planning services through the publicly funded health care safety-net, which is comprised of a variety of providers such as federally qualified health centers (FQHCs) and look-alike clinics, state and local health departments, the Indian Health Service, and specialized family planning clinics. Nationally, more than four in ten (43%) reproductive age women with Medicaid coverage had their last contraceptive visit at a safety-net clinic. This varies widely though, and in some states safety-net clinics play a larger role (Figure 5).
Federally Qualified Health Centers
Under Section 330 of the PHSA, the Health Resources and Services Administration (HRSA) administers federal grants to Federally Qualified Health Centers (FQHCs) whose main focus is providing primary and preventive care to populations that are underserved and predominantly low-income. FQHCs are required to provide “voluntary family planning” services along with a wide range of health care services, but they do not necessarily specialize in providing sexual and reproductive health care. Although it is not specifically defined in FQHC guidelines, voluntary family planning services can include contraceptives, screening and treatment of STIs, pre-pregnancy care and fertility counseling but the range of services that health centers offer can vary. FQHCs must have a sliding fee scale for patients with incomes below 200% FPL and offer services to all patients regardless of their ability to pay.
Specialized Family Planning Clinics
Specialized clinics such as Planned Parenthood centers focus on family planning and reproductive health care, typically offering the full range of contraceptives and other sexual and reproductive health services such as STI testing and treatment, cervical cancer screenings, and pregnancy testing. These clinics also employ clinicians and staff with expertise in family planning care. Planned Parenthood clinics comprise a relatively small portion of clinics that receive public financing for family planning services but have historically served a disproportionate share of safety-net patients (Figure 6).
Health Departments
State and local health departments offer public health services such as vaccines and chronic disease screenings to people who are low-income or uninsured. In many communities, they also offer family planning services, such as HPV vaccines and a limited range of contraceptive services. State and local health agencies may incorporate family planning counseling and services as part of other core public health functions, particularly maternal and child health programs.
Indian Health Services (IHS) Clinics
The Indian Health Service (IHS), an agency under the Department of Health and Human Services, provides a wide range of health services to approximately 2.8 million American Indian and Alaska Native (AIAN) individuals via a network of hospitals, clinics and health stations. Federal regulations require IHS to cover health promotion and disease prevention services, which include family planning services and STI services. However, the availability of contraceptive methods varies by clinic. Services at IHS and tribal clinics are provided with no cost-sharing and are generally only available to members or descendants of federally recognized Tribes who live on or near federal reservations.
Future of Public Financing for Sexual and Reproductive Health
Over the next few years, a confluence of policy changes at the federal level will challenge the network of publicly supported programs and clinics that provide access to free and low cost family planning services. The 2025 Budget Reconciliation law blocks Planned Parenthood clinics from receiving federal Medicaid payments for one year, cutting off a primary source of revenue from a major provider of sexual and reproductive health care for people with low incomes. Additionally, the President and other Republican leaders have proposed eliminating funding for the Title X program. Yet, the Congressional Budget Office estimates an increase of 10 million uninsured individuals over the next decade from the Budget Reconciliation law and the sunsetting of supplemental ACA premium tax credits at the end of 2025 could raise this number even further. With a steep rise in the number of uninsured people, clinics will likely face higher demand in the aftermath of sharp decreases in financing, greatly challenging an already fragile reproductive health safety net.